The Purpose of the CMS 1500 Claim Form
 The CMS 1500 claim form is specifically designed to facilitate the billing process between healthcare providers and insurance companies. It serves as a standardized document to record and submit payment requests for medical services rendered to patients. This form is accepted by various insurance carriers, including Medicare and Medicaid.
The CMS 1500 claim form is specifically designed to facilitate the billing process between healthcare providers and insurance companies. It serves as a standardized document to record and submit payment requests for medical services rendered to patients. This form is accepted by various insurance carriers, including Medicare and Medicaid.
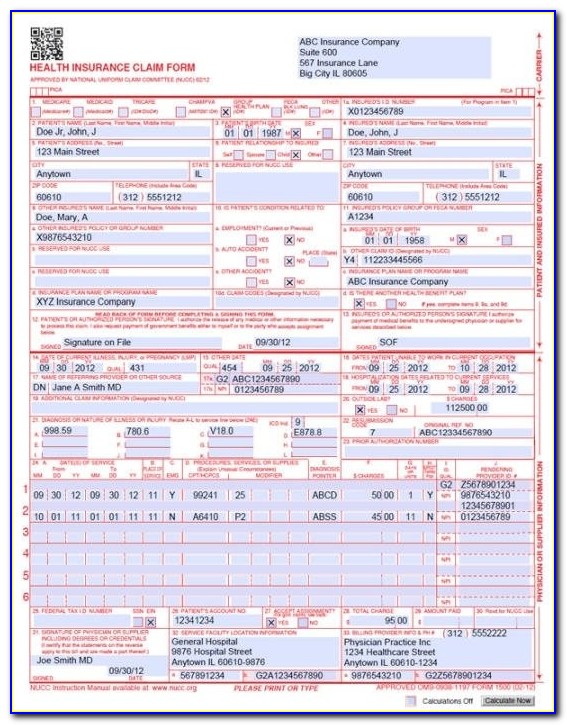
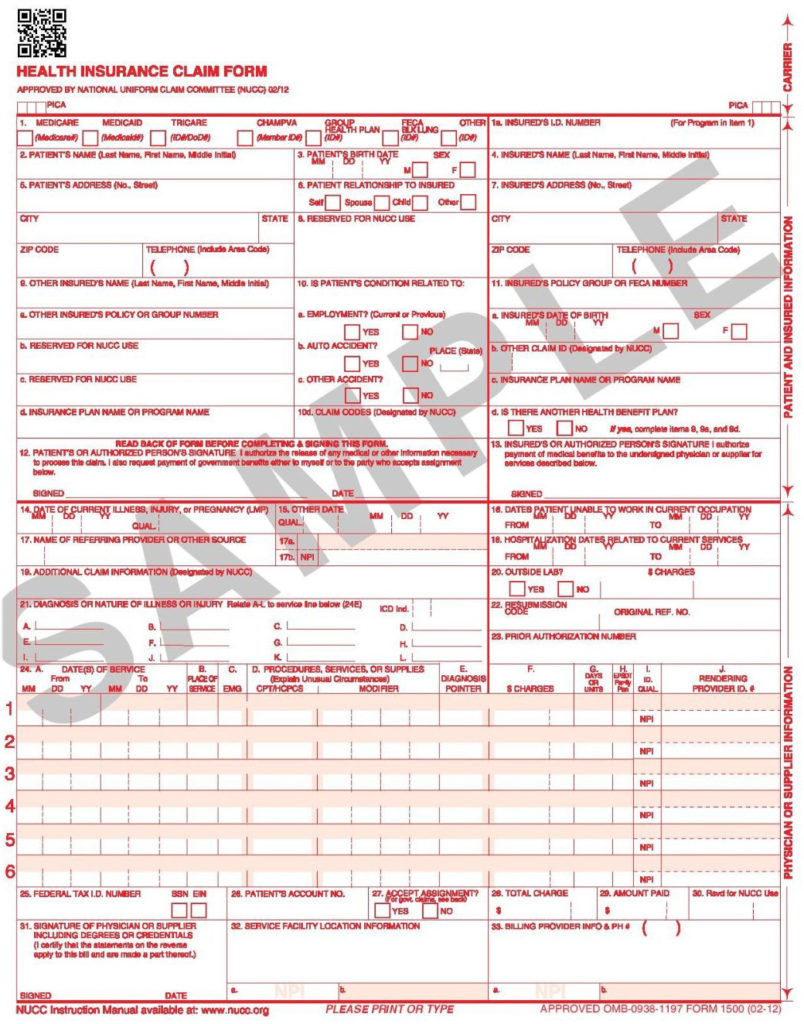
Understanding the Components of the CMS 1500 Claim Form
 To effectively fill out the CMS 1500 claim form, it is crucial to understand its various components. Here are the key sections you need to be aware of:
To effectively fill out the CMS 1500 claim form, it is crucial to understand its various components. Here are the key sections you need to be aware of:
1. Patient Information
The first section of the form requires you to provide detailed patient information, including their name, address, date of birth, and insurance details. It is essential to double-check this information for accuracy to prevent any claim processing delays.
2. Provider Information
In this section, you will input your practice’s details, such as name, address, and National Provider Identifier (NPI) number. Ensure that your information is up to date and matches the records of your contracted insurance companies.
3. Type of Insurance Coverage
Here, you will specify the patient’s insurance coverage, including primary, secondary, or tertiary insurance. This helps the insurance company determine the order in which claims should be processed.
4. Diagnosis and Procedure Codes
Accurate coding of diagnoses and procedures is crucial for claims processing. You will use the International Classification of Diseases (ICD) codes to indicate the patient’s diagnosis and Current Procedural Terminology (CPT) codes to describe the services provided.
5. Billing Information
In this section, you will enter the details of the services rendered, including the date, place of service, and the charges associated with each service. Make sure to calculate and document the charges accurately for proper payment processing.
6. Signature
Finally, the CMS 1500 claim form requires the signature of the physician or authorized healthcare provider. This signature certifies that the information provided is accurate to the best of their knowledge.
Filling Out the CMS 1500 Claim Form
 Now that you understand the various components of the CMS 1500 claim form, let’s dive into the steps to correctly fill it out:
Now that you understand the various components of the CMS 1500 claim form, let’s dive into the steps to correctly fill it out:
Step 1: Gather Patient and Provider Information
Collect all necessary patient and provider information, including names, addresses, phone numbers, and insurance details. Make sure to verify the accuracy of the information before proceeding.
Step 2: Identify Coverage Type
Determine the patient’s insurance coverage type (primary, secondary, or tertiary) and ensure you have the required insurance policy information.
Step 3: Code Diagnoses and Procedures
Using the appropriate diagnosis and procedure codes, accurately document the medical services provided to the patient.
Step 4: Fill in Billing Information
Record the details of each service rendered, including dates, place of service, and associated charges. Double-check the accuracy of the billing information to prevent any processing errors.
Step 5: Obtain Provider Signature
Once all the necessary information has been accurately entered, obtain the signature of the physician or authorized provider. This signature ensures the validity of the claim and certifies its accuracy.
Tips for Successfully Completing the CMS 1500 Claim Form
 While filling out the CMS 1500 claim form, keep the following tips in mind to ensure a smooth claims submission process:
While filling out the CMS 1500 claim form, keep the following tips in mind to ensure a smooth claims submission process:
1. Use Electronic Submissions
Consider electronically submitting your claims whenever possible. Electronic claims are processed faster and reduce the chances of errors or lost paperwork.
2. Double-Check Accuracy
Thoroughly review each section of the form before submission. Verify that all information, including patient demographics, codes, and charges, is accurate and up to date.
3. Follow Guidelines for Specific Fields
Pay attention to specific guidelines and requirements for each field on the CMS 1500 claim form. Incorrectly completed fields can lead to claim rejections or delays in payment.
4. Use Clear and Specific Information
Ensure that all information provided on the form is clear, legible, and specific. Vague or incomplete information may result in claim denials or requests for additional documentation.
5. Keep Documentation for Reference
Make copies of all submitted CMS 1500 claim forms for your records. This documentation can serve as evidence in case of claim disputes or audits.
Conclusion
 Mastering the art of correctly filling out the CMS 1500 claim form is essential for healthcare providers. By understanding the purpose, components, and proper completion of this form, you can streamline your claims submission process and facilitate timely reimbursements.
Mastering the art of correctly filling out the CMS 1500 claim form is essential for healthcare providers. By understanding the purpose, components, and proper completion of this form, you can streamline your claims submission process and facilitate timely reimbursements.
Remember to stay updated with any changes or updates to the CMS 1500 claim form guidelines to ensure compliance with insurance carrier requirements. With accurate and detailed documentation, you can maximize your chances of successfully receiving reimbursements for the medical services you provide.
If you have any further questions or concerns regarding the CMS 1500 claim form, consult with your practice’s billing department or seek guidance from industry experts.